CHAPTER 1
Hospital System Transformation
Systemic service design aiding a healthcare system to listen deeply to its community and foster systemic change in care delivery
Area
Healthcare, Systems Transformation
Role
Client
Contract Health Design & Jr. Data Humanist
St.Paul’s Hospital
Employer
Coeuraj
Duration
2021 - 2022
Impact
Academic paper published based on this work
Fostered healthier community relationships
This work was pivotal in winning a multi-million dollar Engineers Canada RFP
Challenge
Use a collaborative design approach to transform a hospital’s entry experience to become safe and welcoming for a diverse community by engaging stakeholders in a co-design process.
Context
St. Paul’s hospital is a Catholic hospital situated in Saskatoon, the biggest city in Saskatchewan. Its history is one steeped in colonization which has created a complex relationship with the community it serves. A couple years ago, the hospital found itself directed by an emergent thinker, someone who was willing to put in the work to bring about a new role for the hospital in the community. Coeuraj, the consultancy I worked for, was brought in to help the hospital and its staff, go on a transformational journey to begin work on a new health-promoting front-entry experience.
This project began in the second year of COVID-19 pandemic and was underway when the unmarked graves from the residential schools were discovered. On top of this, the weather was reaching highs of 40 degrees celsius and hospital staff were experiencing unprecedented burnout and exhaustion.
To address these additional system drivers and conditions, we adopted a variety of lenses and practices such as trauma-informed care, anti-racism, decolonial and health promotion. We needed to prepare ourselves to enter into this space with high levels of sensitivity, care and consideration for any unintended consequences and to not generate further trauma within the community.
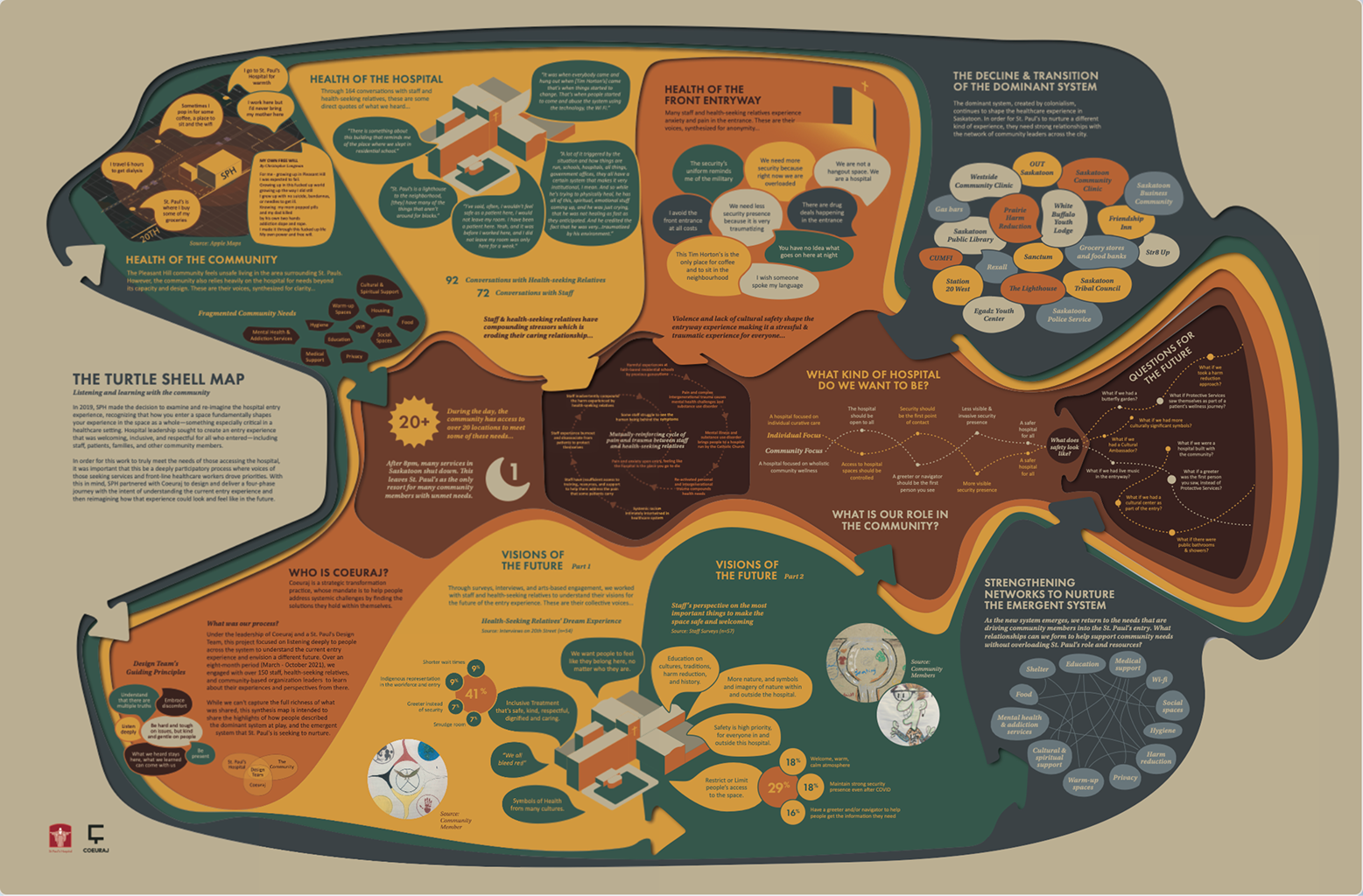
As a contract Health designer on our small, 2-person research and data science team, I was brought in to co-lead the research, design, and execution of the mixed-method participatory research and system mapping with the community. I conducted primary and secondary research, facilitated workshops, built journey maps, mapped the systems at play, then synthesized all the data into system artifacts for leadership level strategic decision making. We engaged with over 160 stakeholders including Indigenous populations, marginalized community members, hospital staff and more.
Phases
Phase 1 - Establishing context & problem mapping
Phase 2 - Digging in & visualizing mental models
Phase 3 - Final artifact & report delivery
Establishing context & problem mapping
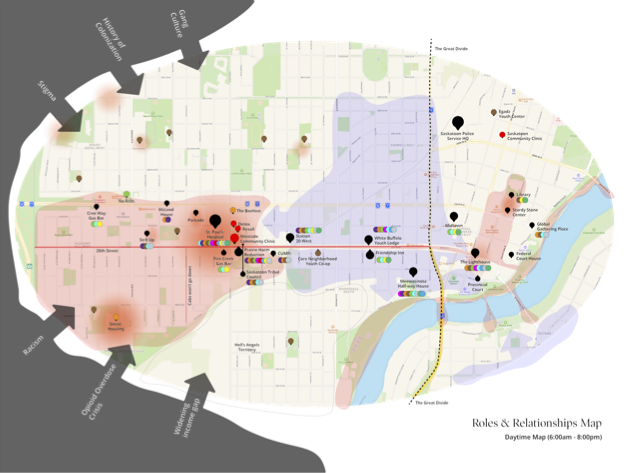
We began our research by focusing on two areas, context and content. This is a cumulative research approach so as to look at things as a whole and not just its parts. I conducted primary and secondary research to uncover socio-political context, community lived-experience, and hospital’s role in the city. We interviewed healthcare professionals, community leaders, general populations, marginalized populations and Indigenous communities to build several maps including actors map, geo-political maps and the day/night services maps which can be seen below.
Day/Night Services Mapping
After several contextualizing interviews we began to notice a pattern in the stories we were hearing. Many of the negative experiences at the hospital were occurring at specific hours of the day. I designed a workshop to clarify this pattern more clearly by co-mapping with participants the dynamics of the community based on the city layout. What this meant when we showed it to the hospital leadership team was how vital the hospital became for the community after 5pm as it was the only place open that could provide shelter, food, wifi and hygiene.
Insight
The area around the hospitals did not provide the services required by the community. This made visible the mental model difference that was creating the tension with the community members, what was considered a health need? If it wasn’t registerable the hospital did not consider it but for the community shelter, food and hygiene are and they should be able to get care from the hospital right?
Digging in & visualizing mental models
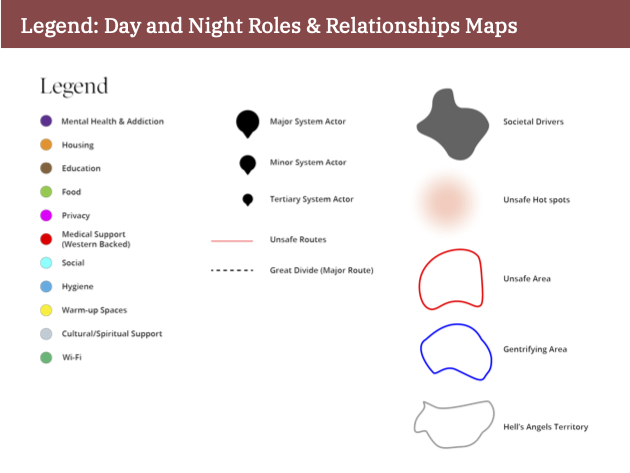
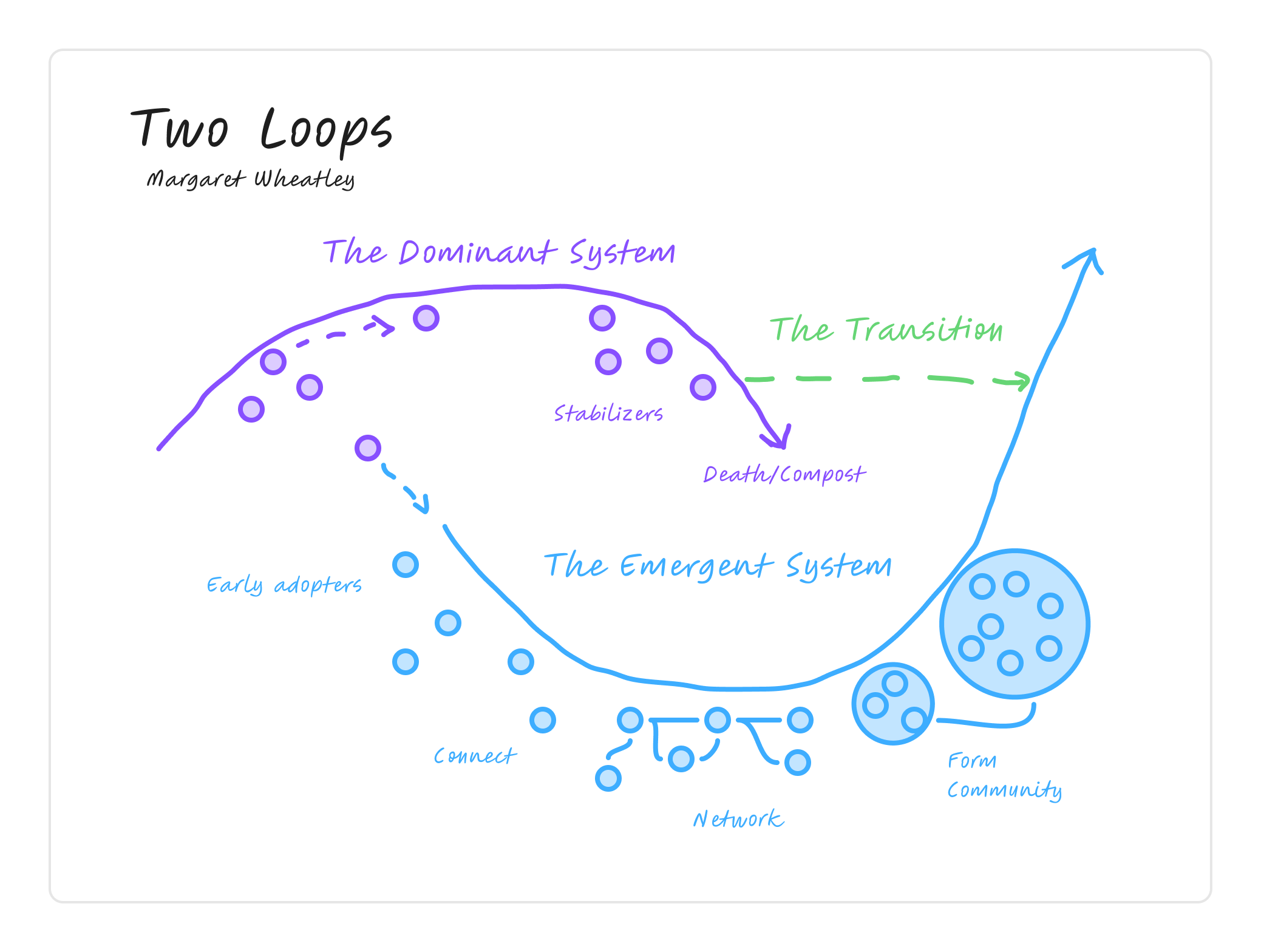
Using foresight techniques such as 3-horizons in combination with Donella Meadow’s leverage points model, Ibram X. Kendi’s Anti-racist model, Shawn Wilson’s research paradigm, and Dave Snowden’s Cynevin framework, we conducted workshops bringing together communities with decision-makers to uncover the impact of registered versus unregistered needs. The workshops were mainly held digitally in Miro but also took place in situ with the hospital’s artist in residence using an arts-based research approach to engage even more of the community.
Co-creating language for systemic change
As we were unpacking the words “patient” and “Unregistered/registered” we began to realise the power of the language choice. During our entire research process we engaged with over 160 voices from the community and hospital staff, listening deeply to not only what they were saying but also how they were saying it. Building off the work of Dr. Pennebaker in psycholinguistics and using our own bespoke pre-LLM tool, we looked at the language use and mapped it against our various frameworks to better understand where the various actors in the system were in terms of thinking beyond western practices of care. We also then began the process of co-creating new language with the community to replace the idea of registered and unregistered health needs as a design intervention.
Insight
Fundamental mental model mismatch between the hospital with registered health needs vs. community health needs, particularly with security and the community.
Final artifact & report delivery
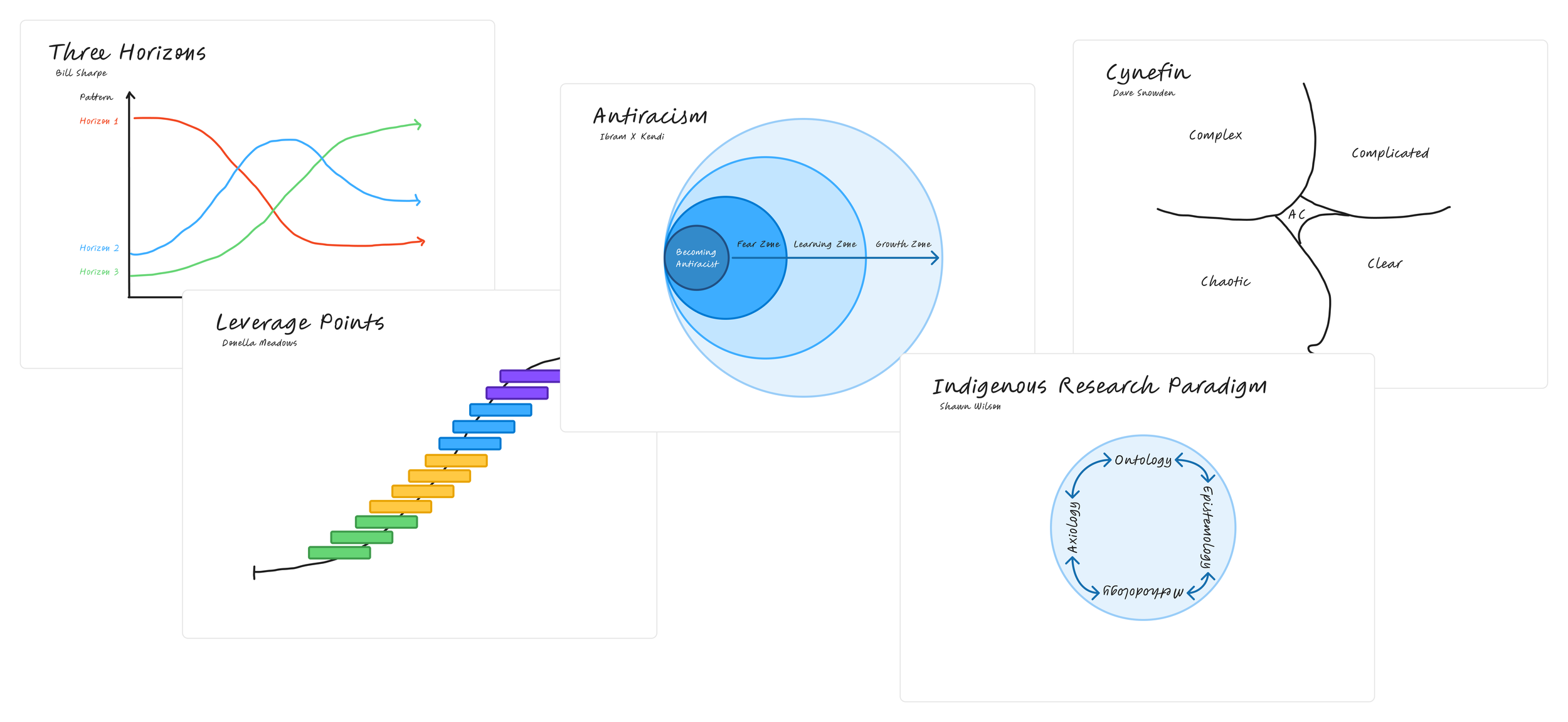
Based on the community engagements, I synthesized thousands of lines of conversation, community art, and lived experience with quantitative data from the hospital into a system map artifact (see below) and results for the accompanying report. The map uses Margaret Wheatley’s two loops model as the base, layering on various pieces of information to describe the impact of the current care practices and elevate community desires as possible intervention points.
Facilitating new language and new relationships
“Health seeking relative”, this is the term that emerged out of our workshops with the community and hospital staff. This new language allowed us to engage all stakeholders in a new kind of conversation, one that was more welcoming, inclusive and health promoting. It then became the central to a positive mental model shift for the security staff who stated in our workshops how it had changed how they view the folks coming into the space. The hospital reported back to us a year later saying how they continue to use this new term and that our work helped spur the hospital towards more inclusive healthcare practices.
Impact
This work was extremely well received by the client and decision-makers now had the data they needed to influence new relationships and move towards new care pathways.
Reflection
This project stood as a pivotal point in my career as a designer. I was able to use all that I had learned and collaborate with my co-workers to develop something unique. I had not know the power that language could play in helping to navigate mental models. It completely changed how I viewed design and the role it can play in creating the right conditions for new relationships to develop.
I also had the wonderful privilege of beginning my work with two incredible people, Angie and Michele. The three of us would go on to move this work forward in the coming years as collaboration science.